ADHD rarely shows up alone. More often, it's part of a bigger picture, sharing symptoms and co-existing with other mental health conditions. This overlap can blur the lines, making it tricky to know what's really going on. Let's explore some of the most common overlaps, what research tells us, and why recognizing them matters.
One of the most common overlaps in adult ADHD is with depression. On the surface, they can look strikingly similar: difficulty concentrating, low motivation, trouble starting or finishing tasks, poor sleep, and feeling overwhelmed.
Research shows that individuals with ADHD are significantly more likely to experience major depressive disorder across their lifespan compared to the general population [1]. The relationship appears to be bidirectional: ADHD symptoms (like procrastination, missed deadlines, or strained relationships) can fuel feelings of failure and hopelessness, while depression's fatigue and negative self-talk can mimic ADHD inattention [2].
Distinguishing them requires looking at onset and course. ADHD inattention usually appears in childhood, whereas depressive cognitive symptoms follow mood changes later in life. Treatment is most effective when both conditions are addressed together, since unrecognized ADHD may blunt antidepressant response [3].
Yet another common overlap is with anxiety, which affects adults with ADHD at much higher rates than the general population [4]. Both bring restlessness, racing thoughts, and sleep problems, but their roots differ. Anxiety is fueled by fear of negative outcomes, while ADHD inattention and impulsivity stem from executive dysfunction.
This overlap can create a vicious cycle: anxious overthinking worsens ADHD distraction, and ADHD-related slip-ups trigger more worry. Research suggests the best outcomes come from treating both using therapy to challenge anxious thought patterns while building ADHD-friendly routines, reminders, and step-by-step planning [5]. Recognizing the overlap is key to breaking the cycle of stress and inattention
In trying to manage distractibility and emotional storms, some adults with ADHD turn to substances for relief. Over time, this can develop into substance use disorders (SUDs).
Research shows that ADHDers are more likely to develop SUDs compared to those without ADHD [6], with heightened risks particularly for nicotine, marijuana, and alcohol use. The challenge is that substance use can briefly mask ADHD symptoms while ultimately worsening impulse control and emotional regulation. This makes treatment complex, underscoring the need for integrated care that addresses both ADHD and SUD together.
High rates of impulsivity, emotional dysregulation, and rejection sensitivity help explain why ADHD and personality disorders (PDs) often co-occur [7]. For some, this overlap means acting without forethought, struggling to regulate emotions, and experiencing deep distress from perceived rejection that can complicate relationships and daily functioning. But this is both a sensitive and less studied area of research so bear in mind that this doesn't mean that all or majority of individuals with ADHD have PDs.
Many adults with ADHD are first diagnosed with anxiety, depression, or other disorders because ADHD symptoms are masked or misinterpreted. Either ADHD is missed, or treatment focuses only on the comorbid disorder leaving ADHD untreated. When ADHD remains undiagnosed, treatments may only partially work, leaving people feeling stuck. That's why raising awareness of ADHD in families, schools, and workplaces, and encouraging early screening is so crucial.
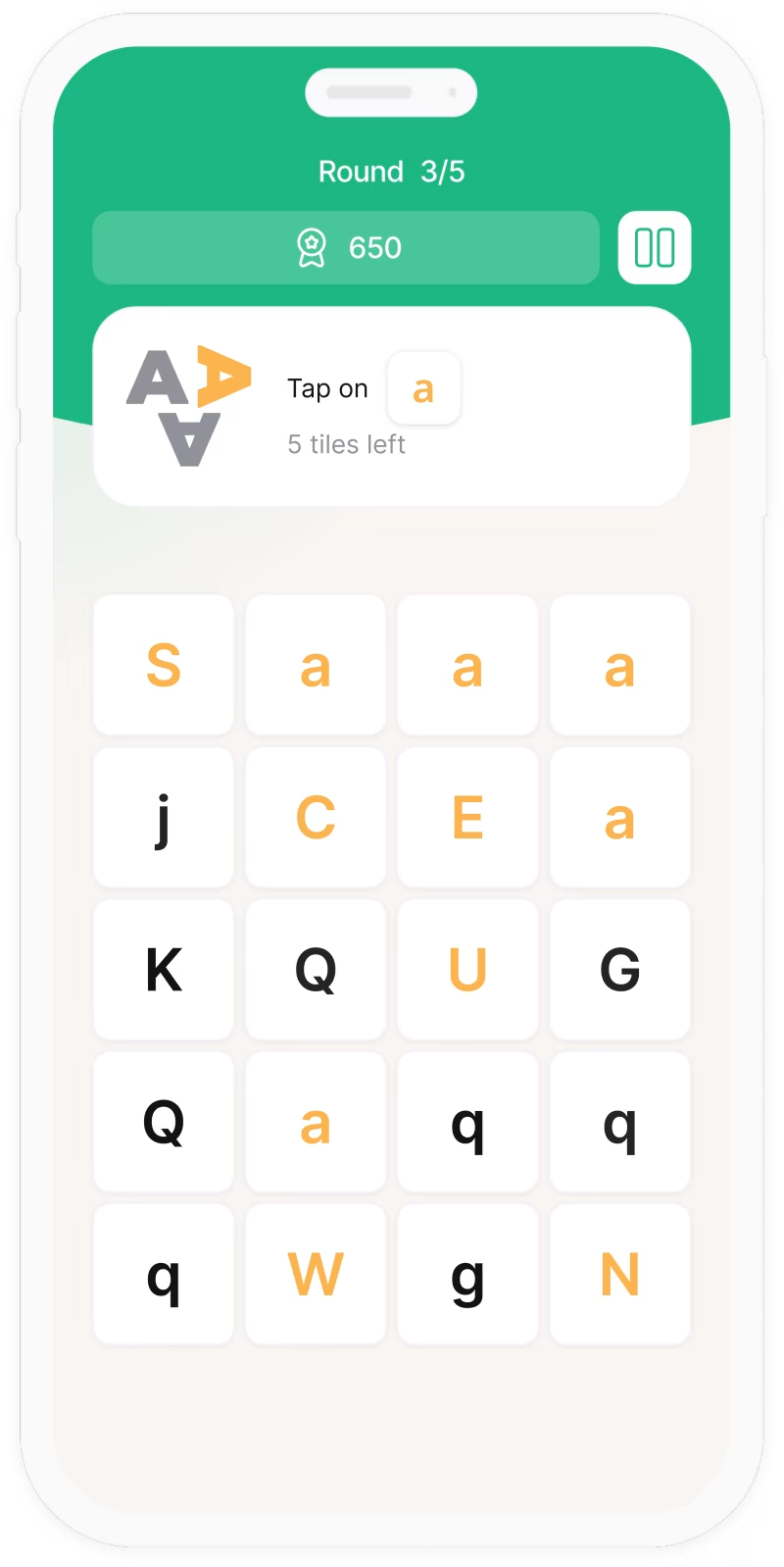
Whether you're here to focus better, calm your mind, or just feel a little more in control, we’re here to support you. One game at a time.